Niger J Paed 2014; 41 (4): 383 - 385
CASE
REPORT
Atimati AO
Hepatoblastoma in an
Abiodun PO
Obaseki DE
adolescent girl: A case report
Olubor OO
DOI:http://dx.doi.org/10.4314/njp.v41i4,18
Accepted: 24th July 2014
Abstract Hepatoblastoma
is the
associated with a poor prognosis.
most common primary malignant
We
report the case of a sixteen
Atimati AO (
)
hepatic tumour in children, occur-
year old girl who presented with
Abiodun PO
abdominal pain and distension and
Department of Child Health
ring between the ages of 6months
to
3years. It most often presents
jaundice of a short duration. She
Obaseki DE
with a painless abdominal mass
was well-nourished with marked
Department of Pathology
discovered accidentally in young
hepatomegaly and ascites. Hepatic
College of Medical Sciences,
children. Occurrence in adoles-
transaminases were highly ele-
University of Benin,
cents and adults is rare and is usu-
vated with deranged clotting pro-
PMB
1154,
ally
associated with non-specific
file. She developed features of
Benin City, Nigeria
symptoms which often result in
hepatic encephalopathy and died
Email: tonyatimati@yahoo.com
delayed diagnosis and commence-
on
the seventh day of admission. A
Post-mortem histologic diagnosis
Olubor OO
ment of treatment. Abdominal
Department of Child Health,
pain preceding a rapidly progres-
of
hepatoblastoma was made.
University of Benin Teaching Hospital,
sive abdominal mass is a common
Benin City,
pattern observed in adolescents
Key words: Hepatoblastoma,
Nigeria.
and
adults. The histologic type
adolescent, poor prognosis
commonly seen in adults is
Introduction
There is paucity of literature on hepatoblastoma in Nige-
ria. A report of primary malignant tumours of the liver
Hepatoblastoma is a rare malignant tumour originating
in
Enugu from 1999 – 2005 showed no case of hepato-
blastoma
out of 424 patients reviewed . Hepatoblastoma
5
in
the cells of the liver . It is the most common primary
1
malignant tumour of the liver in children accounting for
is
rare in adolescents and adults and when it occurs, the
symptoms are usually non-specific . Symptoms associ-
6
about 79% of liver cancer in children in the United-
States . Hepatoblastoma has an annual global incidence
2
ated with adult hepatoblastoma in a review of literature
by
Zheng et al include failure to thrive, rapidly expand-
6
of
0.5 – 1.5 per million in the paediatric population . A
3
review of 274 children with primary malignant hepatic
ing upper abdominal mass, abdominal pain, vomiting
tumours in South Africa from 1988 – 2006 showed a
and fever. In two other case reports abdominal pain
48% prevalence of hepatoblastoma, 27% hepatocellular
which preceded a rapidly expanding upper abdominal
mass was the main presentation .
7,8
carcinoma while vascular tumours, liver sarcomas and
endodermal sinus tumours constituted 25% . The inci-
4
We
present a case of a sixteen year old girl who
dence of hepatoblastoma is highest in infants and falls
presented with a short history of abdominal pain and
off rapidly, with most cases occurring prior to five
swelling and died a week later.
years . There is a higher male to female ratio and white
2
children are often more affected than Negroed children.
1
Case
The aetiology of hepatoblastoma is not quite known, but
cytogenetic abnormalities which include gain of chro-
GL
was a sixteen year old girl referred to our hospital
mosome 2, 8, 20, decreased expression of the adenoma-
with complaints of abdominal pain of 9days and ab-
tous polyposis coli gene and increased expression of β -
dominal
swelling of 8days duration. The pain was dull
catenin have been described in hepatoblastoma . In-
2
aching, located in the right hypochondrium, severe and
creased incidence has been reported in Beckwith-
associated with backache. Pain was present most of the
Weidemann syndrome, hemi-hypertrophy, familial ade-
time. A day after the onset of abdominal pain, she no-
nomatosis polypi and in children with low birth weight .
2
ticed a swelling in the right hypochondrium which was
Infants and younger children with hepatoblastoma typi-
small initially, but progressively increased in size, ex-
cally present with an asymptomatic abdominal mass,
tending to the epigastric and right lumbar regions. There
and diagnosis is often made late, when the disease is
was associated early satiety. There was no fever or vom-
metastatic . The tumour is mainly unifocal, affecting the
3
iting. Patient’s father and mother died 16years and
right lobe more commonly than the left, and occasion-
3years earlier, respectively, from an unknown cause.
ally affects both lobes. Less common features of hepato-
Examination revealed a well-nourished (weight 59kg,
blastoma are weight loss, anorexia and pain .
2
height 1.52m) female adolescent, who was slightly
384
jaundiced, conscious and well-oriented. The abdomen
with
accidental palpation of the liver by caregiver or
was
distended with an abdominal girth of 77cm. The
during routine medical examination.Abdominal pain,
liver was palpable 16cm below the right costal margin
which is a prominent symptom in adolescents and
with a span of 26cm. The liver was tender, firm, with a
adults, usually precedes a rapidly expanding abdominal
mass
7,8,10
smooth surface and well-defined edge. There was mod-
.
Other symptoms include abdominal disten-
erate ascites demonstrable by shifting dullness. She was
sion, weight loss, anorexia, vomiting and fever. Our
tachynoeic and dyspnoeic with normal percussion notes
patient presented with abdominal pain which was
and
breath sounds.
followed shortly by abdominal distension which pro-
Investigations done included: HBsAg (positive), HCV
gressively increased in size.
(negative), prolonged Prothrombin time and Activated
partial thromboplastin time; Total Serum bilirubin
The diagnosis of hepatoblastoma is usually made by
3.5mg/dl, conjugated 1.6mg/dl; normal chest radio-
histology of liver biopsy. Supportive investigations in-
graph; abdominal ultra-sonogram which showed mark-
clude assay for α -fetoprotein, abdominal ultrasonogra-
edly enlarged liver with heterogenous parenchymal
phy, computerized tomography and magnetic resonance
echotexture, smooth outline without a focal mass lesion.
imaging. We did not assay for α -fetoprotein and the diag-
LFT
revealed markedly elevated ALP (689IU/L), AST
nosis was missed by abdominal ultrasonography as has
been similarly reported by Al-jiffry in Saudi Arabia
6
(856IU/L), and ALT (294IU/L).
where the diagnosis was missed both with Ultrasound
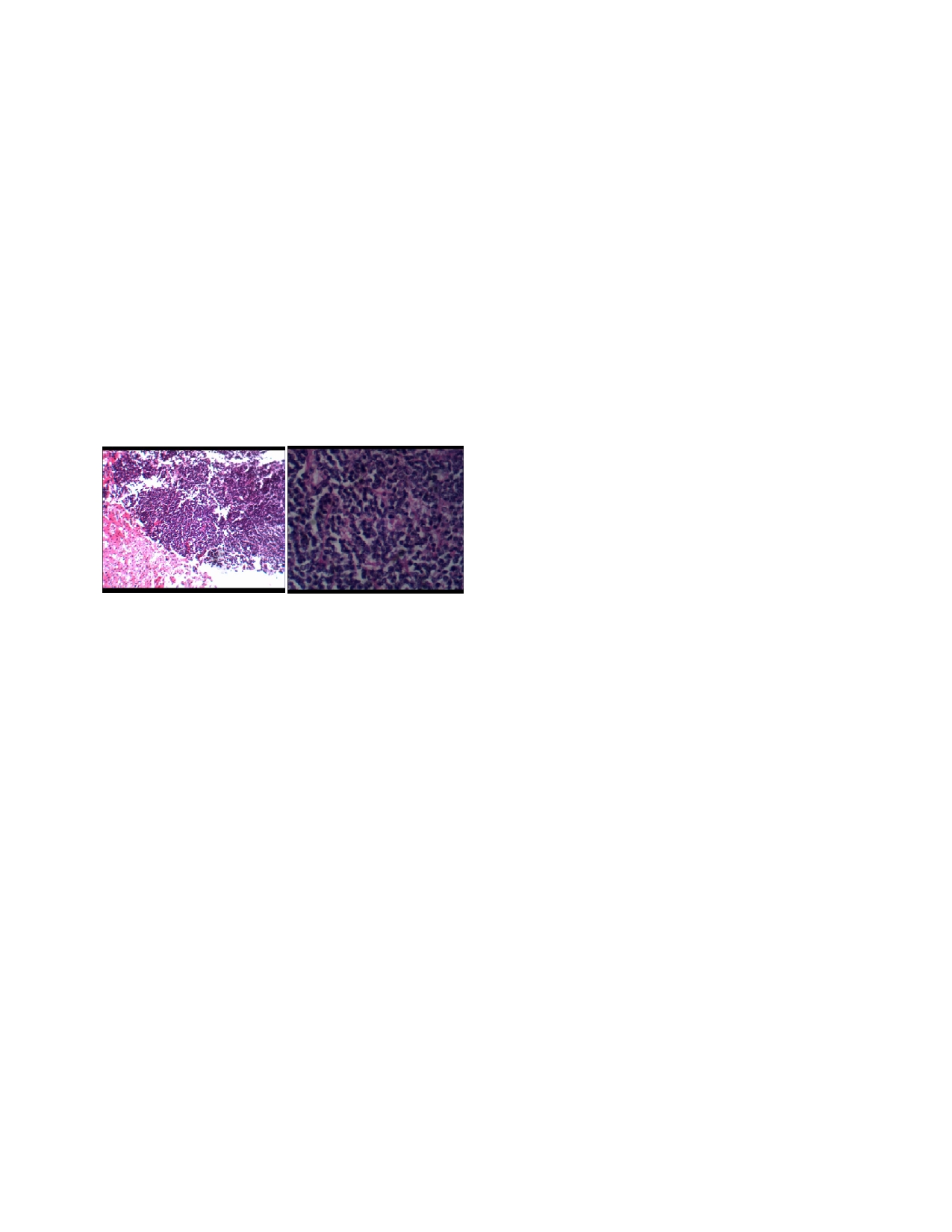
Fig 1a: (H&E
X4) and
1b (H&E
X40) shows
sheets and
rib-
and Computerized Tomography. The tumour is seen as a
bons of small ‘embryonal’ type cells with high nucleo-
hyperechoic,
solid, intra-hepatic mass on abdominal
cytoplasmic ratio, nuclear hyperchromasia and small amount
ultrasound . There is no uniform report on the levels of
11
of
basophilic cytoplasm.
hepatic transaminases in patients with hepatoblastoma.
The markedly elevated hepatic transaminases in this
patient are at variant with the case reported by Al-Jiffry
with normal levels. This difference might be due to the
stage of the disease which is usually done at the time of
surgery. We, however, did not have the benefit of stag-
ing this patient’s disease since the relatives objected to
autopsy. Inagaki et al similarly reported slightly elevated
hepatic transaminases in an eighteen year old male adult
in
Japan .
10
A
diagnosis of Fulminant hepatic failure with a differen-
tial of Hepatocellular Carcinoma was made. She was
A
positive Hepatitis B surface antigen test in this patient
commenced on vitamins A, D, E and K, Neomycin, lac-
is
an unusual finding in Hepatoblastoma. Hepatoblas-
tulose and Dextrose infusion. She also received fresh
toma as often seen in children occurs almost always in
frozen plasma with a view to doing a liver biopsy. Pa-
patients with no underlying liver pathology . This is,
12
tient continued to deteriorate becoming more dyspnoeic
however, different in cases reported in adults where
and restless, with increasing abdominal girth, progres-
there could be co-infection with Hepatitis B as in this
sion of pedal oedema, deterioration of her mental state
patient
3,10
.
Similarly, fibrosis or cirrhosis has been ob-
and worsening clotting profile. She died on the seventh
served in adult cases of hepatoblastoma . This has led
3,6
day on admission. A post-mortem needle biopsy was
to
the consideration that hepatoblastoma may have a
done since relatives did not consent to an autopsy. His-
different pathogenetic pathway in adults compared to
tologic sections of the liver revealed a malignant neo-
children .
6
plastic lesion composed of dis-cohesive sheets of fairly
uniform small cells with scant cytoplasm.
The
cells
The
diagnosis of hepatoblastoma was not a strong con-
have
oval hyperchromatic nuclei with prominent nucle-
sideration in this patient until demise. In almost all of
oli
with presence of pseudorosettes which are consistent
the
cases reviewed by Zheng et al, the diagnosis of
4
with
embryonal histologic type of hepatoblastoma.
hepatoblastoma was not made until histology of the liver
biopsy was received. This is usually due to the older age
of
the patients in which hepatoblastoma is uncommon
and
the unusual mode of presentation. In this patient, the
Discussion
tender hepatomegaly, jaundice, ascites, markedly de-
ranged liver enzymes, prolonged prothrombin and par-
Hepatoblastoma usually occurs between the ages of
tial
thromboplastin time, positive HBsAg, short duration
6months to 3years and the median age at diagnosis is 1
of
symptoms in a well-nourished adolescent led to the
year. Most cases of hepatoblastoma occur before the
9
consideration of fulminant hepatic failure from hepatitis
age
of 5years . Therefore, the occurrence of hepatoblas-
2
B
virus infection as our initial diagnosis.
toma
in this 16year old girl is a very rare occurrence.
Hepatoblastoma is classified by histology as epithelial
Hepatoblastoma has been diagnosed only in a few adults
(56%) or mixed epithelial/mesenchymal (44%). Epithe-
as
shown by a review of all published data and library
lial hepatoblastoma is further divided into pure fetal,
search .
3,6
embryonal, macrotrabecular and small cell undifferenti-
ated types . The embryonal histologic type of
2
Infants and younger children may be asymptomatic ,
3
385
hepatoblastoma found in this patient is usually associ-
Conclusion
ated with a poor prognosis . The purely fetal type
13
which has a
favourable prognosis is rarely found in
Hepatoblastoma is a rare hepatic tumour in adolescents
adult who commonly have the mixed histologic type of
and adults. It often presents with asymptomatic abdomi-
hepatoblastoma . Other prognostic factors outside the
3,6
nal mass in younger children. Abdominal pain is a
histologic type include multiple lobes involvement, de-
prominent feature in adults and usually precedes a
creased p27 gene expression, multi-focal dissemination,
rapidly progressive abdominal mass which often has a
AFP( α -fetoprotein) less than 100 or more than
poor outcome. A high index of suspicion is, therefore,
100,000ng/ml , in addition to late presentation and
14
required to make the diagnosis and institute early treat-
mis-diagnosis which might lead to late institution of
ment.
appropriate treatment. These parameters could not be
evaluated in this patient which, could have contributed
Conflict of interest: None
in
addition to the poor histologic type to the poor prog-
Funding: None
nosis. Complete surgical resection is the mainstay of
treatment of patients with hepatoblastoma. Administra-
tion of chemotherapy enhances complete excision of un-
resectable hepatic tumours
15
which would have been
offered to our patient had the diagnosis been made.
References
1.
Attiveh EF. Hepatoblastoma in
6.
Zheng MH, Zhang L, Gu DN, Shi
11.
De Campo M, de Campo JF. Ul-
children. www.chop.edu/service/
HQ,
Zeng QQ, Chen YP. Hepato-
trasound of primary hepatic tu-
oncology/cancers-explained/
blastoma in adults: a review of
mours in Childhood. Paediatr
diagnosing-and-treating-pediatric-
literature. J
Clin Med
Res 2009;
1
Radiol. 1988; 19(1): 19 – 24.
hepatoblastoma.html.
(1):13 – 16.
12.
Richter A, Grabhorn E, Schulz A,
2.
Herzog CE, Andrassy RJ, Eftek-
7.
Bortolasi L, Marchiori L, Dal
Schaefer HJ, Burdelski M, Gan-
hari F. Childhood Cancers: Hepa-
Dossi I, Colombari R, Nicoli N.
schow R. Hepatoblastoma in a
toblastoma. The Oncologist 2000;
Hepatoblastoma in adult age: a
child with progressive familial
5:445-53.
report of two cases.
Hepatogastro-
intrahepatic cholestasis.
Paediatr
3.
Rougemont A, McLin VA, Toso
enterology 1996;43(10):1073 – 8.
Transplant, 2005;9: 805 – 808.
C,
Wildhaber BE. Adult hepato-
8.
Al-Jiffry BO. Adult hepatoblas-
13.
Haas JE, Muczynski KA, Krailo
blastoma: Learning from children.
toma: A case report and literature
M,
Ablin A, Land V, Vietti TJ.
J Hepatol 2012; 56(6): 1392 –
review. Intl
J Surgery
Case Re-
Histopathology and prognosis in
1403.
ports. 2013; 4(2): 204 – 207.
childhood hepatoblastoma and
4.
Moore SW, Davidson A, Hadley
9.
Schnater JM, Kohler SE, Lamers
hepatocarcinoma. Cancer
GP,
et al. Malignant liver tumours
WH,
von Schweinitz D, Aronson
1989;64: 1082 – 1085.
in
South African children: a na-
DC.
Where do we stand with
14.
Brotto M, Finegold MJ. Distinct
tional audit. World
J Surg.
hepatoblastoma? A review. Can-
pattern of p27/KIP I gene expres-
2008;32(7): 1389 – 95.
cer 2003; 98: 668 – 78.
sion in hepatoblastoma and prog-
5.
Nwokediuko S, Ijoma U, Obienu
10.
Inagaki M, Yagi T, Urushihara N,
nostic implications with correla-
O.
Liver cancer in Enugu, South
Shima Y, Sadamori H, Takakura
tion before and after chemother-
East Nigeria. Insight
Bioinformat-
N,
Tanaka N, Oda M. Successfully
apy. Hum
Pathol 2002;33:198
–
ics
2011;1(1):1 – 5.
resected hepatoblastoma in a
205.
young adult with chronic hepatitis
15.
Pinpalwar AP, Sharif K, Ramani
B:
report of a case. Eur
J Gastro-
P,
Stevens M, Grundy R, Morland
enterol Hepatol 2001; 13(8):981 –
B,
Lloyd C, et al. Strategy for
4.
hepatoblastoma management:
Transplant versus non-transplant
surgery. J
Pediatr Surg
2002; 37:
240 – 245.